Cultural competency is crucial in healthcare, especially for mental health services, as evidenced by Littleton Kaiser Permanente's successful model. Their approach enhances patient engagement and satisfaction through culturally sensitive care tailored to diverse backgrounds, leading to improved access and outcomes. A comprehensive training program should focus on cultural sensitivity, inner strength development, and policy advocacy, enabling providers to overcome biases and advocate for systemic changes in mental healthcare. Regular evaluations, like those assessing the Littleton Kaiser Permanente mental health services number, are vital to ensure these initiatives remain effective, benefiting patients and providers across diverse communities.
Healthcare provider cultural competency training is essential in delivering effective mental health services, as evidenced by the success of programs like the Littleton Kaiser Permanente model. This article explores the significance of cultural competency in healthcare, particularly within mental health care. We delve into a case study showcasing improvements in patient outcomes and provider interactions at Littleton Kaiser Permanente. Additionally, key components of comprehensive training programs and methods for measuring their impact are discussed, highlighting best practices to enhance cultural sensitivity in mental health services.
- Understanding Cultural Competency in Healthcare: Why It Matters for Mental Health Services
- The Littleton Kaiser Permanente Model: A Case Study in Effective Training Programs
- Key Components of a Comprehensive Cultural Competency Training Program
- Measuring Impact: Evaluating the Success of Cultural Competency Initiatives within Mental Health Care
Understanding Cultural Competency in Healthcare: Why It Matters for Mental Health Services
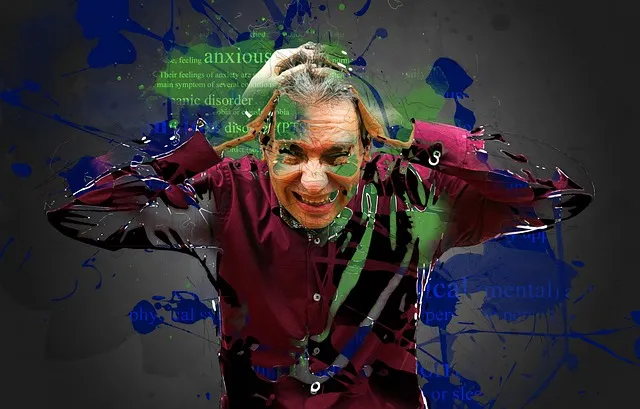
Cultural competency is a vital aspect of healthcare that involves recognizing and respecting the diverse cultural backgrounds and values of patients. In the context of mental health services, this understanding is particularly crucial as it can significantly impact patient care and outcomes. Many individuals from different ethnic and cultural groups may face unique challenges when seeking mental health support. These challenges can range from language barriers to differences in perception and expression of emotional distress.
For instance, a study focusing on Littleton Kaiser Permanente’s mental health services revealed that culturally competent care led to improved patient engagement and satisfaction. The Crisis Intervention Guidance provided by the organization considers various cultural contexts, ensuring that interventions are sensitive to diverse needs. This approach not only facilitates better access to services but also promotes the development of coping skills tailored to individual cultural frameworks, fostering a more inclusive Mental Health Awareness across all communities served.
The Littleton Kaiser Permanente Model: A Case Study in Effective Training Programs
The Littleton Kaiser Permanente Model is a noteworthy case study showcasing how comprehensive cultural competency training can transform healthcare delivery. This pioneering program focuses on empowering medical professionals to offer enhanced mental health services tailored to diverse patient populations. By integrating self-esteem improvement and emotional well-being promotion techniques, the model goes beyond traditional care, addressing the holistic needs of patients from various cultural backgrounds.
The training emphasizes effective communication strategies, equipping healthcare providers with the skills to navigate complex interpersonal dynamics. This approach not only improves patient satisfaction but also fosters more accurate diagnoses and effective treatment plans. The Littleton Kaiser Permanente mental health services number serves as a beacon, demonstrating the positive impact of such initiatives on both individual lives and the broader healthcare system.
Key Components of a Comprehensive Cultural Competency Training Program
A comprehensive Cultural Competency Training Program for healthcare providers should incorporate several key components to effectively address diverse cultural needs within the community. Firstly, it must emphasize Cultural Sensitivity in Mental Healthcare Practice, ensuring that staff are equipped to navigate the intricate web of cultural beliefs and values that influence mental health experiences. This includes training in recognizing and respecting individual and collective identities, understanding cultural variations in communication styles, and learning how to adapt services accordingly.
Additionally, programs should focus on Inner Strength Development among staff. Equipping healthcare providers with tools to manage their own biases and stress responses enables them to create safer, more supportive environments for patients from diverse backgrounds. This aspect of training fosters resilience, enhances self-awareness, and promotes empathetic engagement. Moreover, integrating discussions around Mental Health Policy Analysis and Advocacy into the curriculum empowers staff to contribute to systemic changes that address cultural disparities in mental health care access and outcomes at the community level.
Measuring Impact: Evaluating the Success of Cultural Competency Initiatives within Mental Health Care

Evaluating the success of cultural competency initiatives within mental health care is paramount to understanding their true impact on patient outcomes and provider well-being. At Littleton Kaiser Permanente, for instance, the number of mental health services provided has significantly increased following the implementation of these programs. By assessing key metrics such as patient satisfaction, treatment adherence, and reduction in readmission rates, researchers can gauge the effectiveness of cultural competency training.
Inner Strength Development, a core component of these initiatives, focuses on enhancing coping strategies and stress management techniques among both patients and providers. This not only improves mental health outcomes but also plays a crucial role in burnout prevention. Regular evaluations allow for adjustments to be made, ensuring that programs like these remain relevant and impactful, fostering inclusive care environments where everyone feels valued and supported.
Cultural competency training is a game-changer in mental health care, as evidenced by the successful Littleton Kaiser Permanente model. This case study highlights the significant impact of comprehensive programs on improving healthcare provider understanding and sensitivity to diverse cultural needs. By implementing key components such as community engagement, interactive workshops, and ongoing evaluation, mental health services can become more inclusive and effective for all patients. The number of initiatives focusing on cultural competency within mental health care is growing, demonstrating a crucial step towards enhancing patient outcomes and ensuring equitable access to quality care.